Congestive prostatitisis a disease process in the prostate caused by congestion. The pathogenic flora is not detected; microscopy of prostate secretions, semen and urine may reveal leukocytes. Symptoms include constant pain in the perineum and dysuria. The diagnosis is based on the results of bacterial culture of the biomaterial and TRUS. There is no single treatment regimen for congestive prostatitis: massage, physiotherapy, antimicrobial drugs and alpha-blockers are prescribed. An individual approach is necessary, taking into account the existing symptoms. If conservative treatment fails, surgical intervention is possible.
general informations
Prostatitis can be infectious, caused by the presence of pathogenic microflora, or stagnant, associated with blood congestion, retention of ejaculate and prostate secretions. Congestive or congestive prostatitis (vegetative urogenital syndrome, prostatosis) is an outdated name. Modern specialists in the field of urology more often use the term "chronic pelvic pain syndrome without inflammatory response" (CPPS). Prostatitis occurs in 25% of men aged 35-60 years, inflammation caused by congestive processes accounts for 88-90% of the total number of cases. The potentially congestive form of the disease is favored by pathogens in the L form, fixed on biofilms and not detected by routine methods.
Causes
The causes of congestive prostatitis can be associated both with the gland itself and with extraprostatic factors. The exact etiology is unknown, probably due to stagnation of secretions in the prostate or venous congestion of the pelvic organs and scrotum. Some urologists consider this disease psychosomatic. The border between bacterial and abacterial inflammation is very arbitrary: with immunosuppression of any origin, due to the addition of secondary microflora, the process becomes infectious. Congestive prostatitis is caused by:
- Internal urological causes. Functional or structural pathology of the bladder: cervical obstruction, inability of the external sphincter to relax during bowel movements, impaired detrusor contractility contribute to urinary retention and, due to compression of the vessels, to blood stagnation. Prostate hyperplasia and tumor, urethral stenosis, and obstructive bladder stones are also considered potential causes of venous congestion.
- Compression. Blood circulation is impeded due to compression of the venous plexus by a retroperitoneal tumor, metastases and intestinal loops filled with feces (constipation). The vessels of the genitourinary plexus expand, blood flow slows down, tissues lack oxygen and are replaced by non-functional structures. Some blood is deposited and cut off from circulation.
- Behavioral factors. Refusal of sexual activity, irregular ejaculation and resorting to interrupted sexual intercourse as a means of preventing unwanted pregnancy cause blood flow and swelling of prostate tissue. During ejaculation, this gland is not completely emptied. Constant masturbation can lead to congestive prostatitis, because. . . For the development of an erection, a flow of blood to the genitals is necessary.
Predisposing factors include low physical activity, hypothermia and overheating, poor diet with a predominance of spicy and smoked foods. Alcohol and nicotine affect the tone of the vascular wall, disrupt redox processes and permeability, which causes swelling. The main prerequisites for the formation of congestive prostatitis affecting all organs of the male genital area (vesicles, testicles) are considered to be anomalies of the vascular system of the pelvis - valve insufficiency, congenital weakness of the vein wall.
Pathogenesis
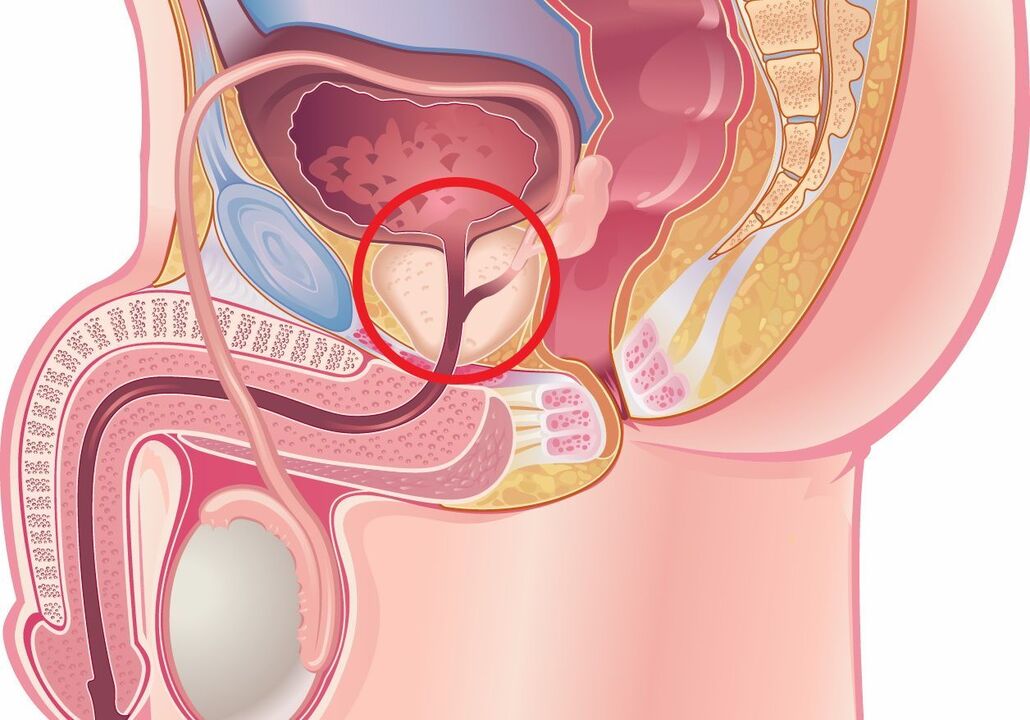
The peripheral zone of the prostate consists of ducts with a poorly developed drainage system, which prevents the flow of secretions. As the prostate enlarges with age, patients develop reflux of urine into the prostate tubes. It has been found that many men suffering from prostatitis are more prone to allergies. Scientists believe that these patients may also suffer from autoimmune inflammation caused by a previous infection.
Urinary reflux is favored by urethral strictures, bladder dysfunction and BPH. Backflow of even sterile urine causes chemical irritation and inflammation. Fibrosis of the tubules is initiated, prerequisites for prostatolithiasis are created, which increases intraductal obstruction and stagnation of secretions. Inadequate drainage of the acini triggers an inflammatory reaction, increased swelling is accompanied by the appearance of symptoms. The condition is made worse by congestion (stagnation) of blood in the pelvis.
Classification
The general classification of prostatitis includes acute (I) and chronic (II) bacterial forms. Category III includes subtype IIIa – CPPS with inflammation and IIIb – CPPS without inflammation. Congestive prostatitis is considered a manifestation of CPPS without an inflammatory response (IIIb). There is a clinical differentiation which takes into account the pathogenetic and morphological characteristics of the disease:
- First stage.Characterized by the predominance of the processes of exudation, emigration, arterial and venous hyperemia, leading to damage to the microvascularization and destruction of glandular tissue. These changes are recorded during the first years after the onset of the disease. The clinical picture at the first stage is the most pronounced.
- Second step.The initial processes of connective tissue proliferation develop and symptoms decrease. Due to the formation of thrombus, the microcirculation suffers, which aggravates sclerosis. At this stage, most patients suffer from sexual dysfunction: erection and intensity of orgasm weaken, premature ejaculation develops, or vice versa, the man experiences difficulty achieving orgasm.
- Third step. Severe fibrosclerotic changes are typical. It has been proven that connective tissue proliferation is stimulated not only by inflammation, but also by ischemia that accompanies congestive prostatitis. Complaints about difficulty urinating are typical, and renal involvement in the pathological process is noted.
Symptoms of congestive prostatitis
Pathology manifests itself by a variety of symptoms. Most patients describe the pain as constant discomfort in the perianal area, scrotum, or penis. Some people note an increase in perineal pain when sitting. The irradiation of pain is variable - to the lower back, inner thighs, coccyx. The swelling of the gland often makes it difficult to start urinating and weakens the urinary stream. A type of congestive inflammation against the background of vascular pathology is often accompanied by hemospermia - the appearance of blood in the semen.
Symptoms of bladder irritation include frequent urge and urge urinary incontinence. With long-term pathology, depressive disorders develop. It is still questionable whether psycho-emotional characteristics lead to discomfort in the perineum or, conversely, whether the pain caused by enlarged prostate affects a man's mental state. An increase in temperature accompanied by chills indicates the transition from abacterial congestive prostatitis to infectious prostatitis and the need to begin pathognomonic treatment.
Complications
Congestive prostatitis with added microflora can become acute bacterial. Neighboring organs and structures may be involved in the inflammatory process: vesicles, bladder, testicles. The role of the prostate is to produce fluid for sperm; it normally has a special composition which has a protective function for male germ cells. Insufficient amounts of nutrients and changes in the biochemical properties of prostate secretions inevitably affect the quality of ejaculate; Men with congestive prostatitis are more often diagnosed as infertile.
In case of severe swelling of the organ, part of the urine after urination remains in the bladder, which leads to the formation of pathological reflux of urine into the ureters and the renal collecting system. In response to reflux, hydronephrosis and persistent pyelonephritis with renal failure may occur. 50% of men develop sexual dysfunctions: painful ejaculation, dyspareunia, uncomfortable nocturnal erections, which worsen the quality of life and negatively affect the couple's relationship.
Diagnostic
Determining the origin of symptoms is crucial for the effective treatment of congestive prostatitis, which is why different questionnaires have been developed to facilitate diagnosis: I-PSS, UPOINT. These questionnaires are available in Russified form, they are used by urologists and andrologists in their practice. To exclude myofascial syndrome, a consultation with a neurologist is indicated. On palpation, the prostate is enlarged, moderately painful, the congestive nature of the disease is evidenced by the varicose veins of the rectum. Diagnosis of congestive prostatitis includes:
- Laboratory tests. A microscopic and cultural examination of the prostatic juice is carried out. A slight increase in microscopic leukocyte counts and negative bacterial culture results confirm abacterial congestive inflammation. PCR tests are carried out to exclude the sexually transmitted nature of the disease. In the third portion of urine after massage, more pronounced leukocyturia is detected. To exclude a bladder tumor, urine cytology can be performed; in patients over 40 to 45 years old, a PSA blood test is justified.
- Visual search methods. The main instrumental diagnostic method remains TRUS, ultrasound of the bladder. Cystourethrography findings are informative in confirming bladder neck dysfunction, revealing intraprostatic and ejaculatory reflux of urine and urethral stenosis. In the event of a pronounced weakening of the jet, a flow measurement is carried out. Pelvic floor muscle tension is assessed using a videourodynamic study.
The differential diagnosis is carried out with bladder carcinoma, BPH, interstitial cystitis. Similar manifestations are observed in genitourinary tuberculosis and urethral stenosis, since these nosologies are also characterized by pain in the lower abdomen, symptoms of dysuria and difficulty urinating. Congestive prostatitis is distinguished from bacterial prostatitis and all pathological processes that accompany CPPS in men should be excluded.
Treatment of congestive prostatitis
The patient is recommended to normalize his sex life, because regular ejaculation helps drain the acini and improve microcirculation. Interrupted or prolonged sexual intercourse, causing congestion, is unacceptable. A number of products have been identified that increase the chemical aggressiveness of urine - their consumption leads to an increase in symptoms of congestive prostatitis. Spices, coffee, marinades, smoked foods, alcoholic and carbonated drinks should be limited, or better yet excluded. Treatment of congestive inflammation of the prostate can be conservative and surgical.
Conservative therapy
The treatment regimen is chosen individually, depending on the dominant symptoms. In many patients, improvement occurs after taking antibacterial drugs, which is explained by incomplete diagnosis of latent infections. In case of slow urinary flow and the need to strain, alpha-blockers are prescribed. Urinary urgency is neutralized with anticholinergic drugs. 5-alpha reductase inhibitors have been shown to reduce the severity of clinical manifestations by reducing the response of macrophages and leukocytes and their migration into the inflammatory zone.
Pain relievers, nonsteroidal anti-inflammatory drugs, and muscle relaxants can help relieve pain and muscle spasms. It is reasonable to include in the treatment regimen drugs that normalize microcirculation – phlebotonics (venotonics). If the stagnant process promotes androgen deficiency, they resort to hormone replacement therapy. Patients suffering from anxio-hypnotic and depressive disorders are advised to consult a psychiatrist who will select the optimal antidepressant.
In case of congestive inflammation of the prostate, physiotherapeutic procedures help to normalize men's health. They use laser and magnetic therapy, electrophoresis, etc. Thermal treatments help relieve the symptoms of dysuria and improve sexual function: taking alkalizing mineral waters, applications of paraffin and mud, massaging showers. In some patients, normalization of well-being is noted when carrying out exercise therapy to reduce tension in the pelvic muscles. Prostate massage does not replace natural ejaculation, but improves blood circulation and drainage of the organ.
Minimally invasive treatment methods
If conservative treatment fails, high-tech interventions are considered - transurethral resection of the prostate, ablation with high-intensity focused ultrasound. The most effective is transrectal hyperthermia - a non-invasive method based on the principle of thermal diffusion (the prostate is exposed to unfocused microwave energy). Heat increases tissue metabolism, reduces congestive symptoms and has a neuroanalgesic effect. Data on the effectiveness of treatment procedures for congestive prostatitis are limited.
Prognosis and prevention
The lifetime prognosis is favorable, but chronic pelvic pain is difficult to treat. Sometimes congestive prostatitis goes away spontaneously over time. Prolonged circulatory disorder leads to sclerosis of the glandular tissue, which is manifested by a deterioration in spermogram parameters. The prognosis for congestive prostatitis largely depends on the patient's compliance with all recommendations and lifestyle changes.
Prevention consists of playing sports, avoiding lifting heavy objects, normalizing sexual relations and avoiding the consumption of coffee and alcohol. When working in a sedentary manner, it is recommended to take breaks to do physical exercises and use a pillow. Loose-fitting underwear and pants are preferred. Patients are observed by a urologist with periodic assessment of prostate secretions for inflammation and ultrasound and, if necessary, receive antibacterial treatment and prostate massage sessions.




































